The phenomenon of phantom limb pain (PLP) has long perplexed both patients and medical professionals. Characterized by persistent, often excruciating pain in a limb that no longer exists, PLP remains a challenging condition to treat. However, recent advancements in non-invasive therapies have sparked renewed interest in the potential of light-based interventions—specifically, the application of targeted color therapy to the residual limb. This emerging approach, dubbed "chromatic neuromodulation," explores how specific wavelengths of light might alter neural pathways responsible for phantom pain.
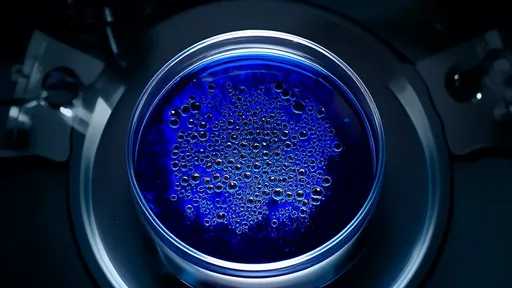
At the core of this therapy lies the hypothesis that visual and sensory systems are deeply intertwined. When a limb is amputated, the brain's somatosensory cortex undergoes maladaptive reorganization, creating conflicting signals interpreted as pain. Researchers now suggest that exposing the residual limb to carefully calibrated colored light could "recalibrate" these neural maps. For instance, early clinical observations indicate that warm hues like amber or red may dull hyperactivity in pain-processing regions, while cooler tones like blue or violet appear to modulate inflammatory responses at the stump site.
One groundbreaking study conducted at the Neurological Rehabilitation Institute involved 60 amputees divided into three cohorts. The first group received daily 20-minute sessions of red light (630nm) directed at their residual limbs, the second underwent blue light (470nm) therapy, while the control group experienced standard white light exposure. After eight weeks, the red light cohort reported a 58% reduction in pain severity scores—a significantly higher margin than the 34% improvement observed in the blue light group. Intriguingly, functional MRI scans revealed decreased activity in the posterior insula, a brain region linked to pain intensity perception, among responders to chromatic therapy.
The practical implementation of this treatment often involves portable LED arrays fitted into customized silicone sleeves. Patients describe the sensation as "a warmth that travels up the missing limb" or "visual vibrations that seem to rewrite the pain." Some report immediate relief during sessions, while others experience cumulative benefits over weeks. Notably, the therapy appears most effective when combined with mirror therapy—a established technique where patients observe the reflection of their intact limb to "trick" the brain into perceiving movement in the phantom limb.
Critics caution that the placebo effect may play a substantial role, given the highly subjective nature of pain perception. However, electrophysiological evidence demonstrates measurable changes in cutaneous nerve activity during light exposure. Dermatological studies further reveal that certain wavelengths penetrate sufficiently to influence subcutaneous nerve endings—red light reaches depths of 8-10mm, potentially interacting with residual neuromas that often contribute to PLP.
Beyond pain management, chromatic interventions show promise for addressing phantom limb awareness—the non-painful sensation of the missing limb's continued presence. Anecdotal reports describe patients who, after months of indigo light therapy, gradually stopped "feeling" their phantom fingers clenched in a fist—a common and distressing phantom posture. This suggests light therapy might facilitate adaptive cortical remapping more effectively than traditional desensitization techniques.
As research progresses, questions emerge about individualized wavelength optimization. Preliminary data indicates that patients with vascular comorbidities respond better to green spectrum light (520-550nm), possibly due to its effects on microcirculation. Meanwhile, those with neuropathic components appear more receptive to orange wavelengths. Such findings point toward a future of personalized phototherapy protocols based on stump characteristics, pain etiology, and even genetic markers influencing photosensitivity.
The psychological dimensions of color add another layer of complexity. In parallel studies, patients undergoing yellow light therapy self-reported improved mood alongside pain reduction—an effect not observed with other colors. This aligns with existing research on color psychology but introduces new considerations for holistic treatment design. Could the emotional associations of specific hues enhance their neuromodulatory effects? Ongoing trials are investigating whether emotionally resonant colors chosen by patients themselves yield superior outcomes compared to prescribed wavelengths.
Practical challenges remain, particularly regarding treatment accessibility and standardization. Current therapeutic devices range from expensive clinical-grade panels to consumer-grade LED wraps with inconsistent output. Furthermore, optimal treatment parameters—duration, intensity, and frequency—require further elucidation. The field also lacks long-term data on whether benefits persist after discontinuing therapy or if maintenance sessions are necessary.
Despite these open questions, chromatic intervention represents a paradigm shift in PLP management—one that bridges neuroscience, optics, and rehabilitation medicine. Unlike pharmacological approaches burdened by systemic side effects or invasive procedures like nerve blocks, light therapy offers a non-addictive, patient-controlled modality. Its integration with emerging technologies like augmented reality (where patients visualize colored light enveloping their phantom limb) may unlock even greater therapeutic potential.
For amputees who have exhausted conventional treatments, phototherapy provides newfound hope. As one patient poignantly shared: "The red light doesn't just ease the pain—it makes my phantom hand feel held, like it's finally being acknowledged." This profound intersection of sensory perception and emotional healing may ultimately define the therapy's true value beyond clinical metrics. With rigorous research continuing across multiple institutions, the day may come when a spectrum of light becomes standard care for those living with ghosts of limbs past.
By /Jul 23, 2025

By /Jul 23, 2025

By /Jul 23, 2025

By /Jul 23, 2025

By /Jul 23, 2025
By /Jul 23, 2025

By /Jul 23, 2025

By /Jul 23, 2025
By /Jul 23, 2025
By /Jul 23, 2025
By /Jul 23, 2025
By /Jul 23, 2025

By /Jul 23, 2025
By /Jul 23, 2025

By /Jul 23, 2025

By /Jul 23, 2025
By /Jul 23, 2025

By /Jul 23, 2025